COVID-19
COVID-19 is an infectious disease caused by SARS-CoV-2. COVID-19 is very contagious and can spread quickly. The best way to prevent illness is to avoid being exposed to the virus. The virus spreads mainly from person to person through respiratory droplets produced when an infected person coughs, sneezes or talks. COVID-19 can be spread by people who are not showing symptoms (asymptomatic). COVID-19 can be diagnosed through testing, and vaccination can help protect you.
Environment, Health and Safety (EHS) has developed the following guidance and resources for the UNC-Chapel Hill community:
Cloth Masks
Cloth masks can be made from a variety of natural and synthetic fabrics and fibers, various types of cloth mask are available. Cloth masks should have:
- Two or more layers of washable, breathable fabrics.
- Nose wire for a snug fit. Make sure the mask is not loose and has no gaps.
- Cloth thick enough to block light when held up to bright light sources.
- Do not wear cloth masks with exhalation valves or vents.
For a better fit and protection, cloth masks can be worn over a disposable mask or combined with a fitter or brace.
Disposable/Surgical Masks
Disposable/Surgical masks are fluid-resistant, loose-fitting protection that provide a barrier between the mouth and nose for the wearer against potential contaminants in the environment.
- Multiple layers of non-woven material
- Nose wire
K95 Masks
K95 masks are filtering facepiece respirators commonly made in China that are like N95 masks used in the United States. Make sure K95s:
- Meet the requirements set by the CDC and National Institute for Occupational Safety and Health (NIOSH).
- Make sure the K95 is not counterfeit (about 60% of K95s in the US are counterfeit and not approved for use, according to the CDC and NIOSH).
- Do not wear more than one K95 at a time, and they should not be worn with facial hair.
N95 Masks for Healthcare Workers
N95 masks are tight-fitted filtering facepiece respirators with protection against airborne particles. N95s come in different makes and models. N95 use should include:
- A fit test, before use, to determine a proper fit.
- Training on how to use N95 properly.
- NIOSH-approved.
- Cover your nose and mouth when wearing the mask.
- Keep your mask clean and dry. Replace if it becomes wet or soiled.
- If the mask is disposable, throw it away after one use.
- Wash your hands or use hand sanitizer before handling your mask.
- Make sure you can breathe easily through the mask.
How to Store and Wash Your Mask
Store your clean dry mask in a breathable bag, such as a paper or mesh fabric bag, to keep it clean between uses. When reusing your mask, keep the same side facing out. Be sure to wash or sanitize your hands when handling your mask.
Wet cloth masks should be stored in a sealed plastic bag until they can be washed.
How to Wash Your Mask
Be sure to keep your mask clean. Cloth masks can be washed using a washing machine or by hand with laundry detergent or soap. Make sure to completely dry your mask using a clothes dryer or through air drying by hanging or laying it flat.
CDC Guide to Masks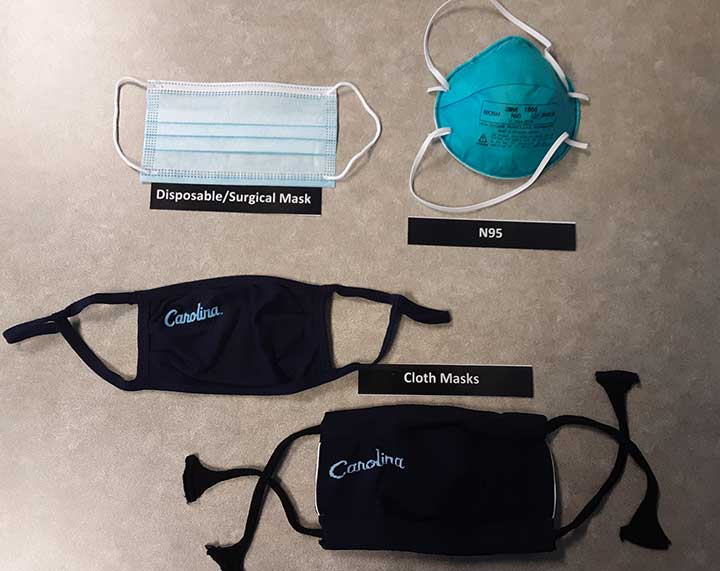
Common Disinfectants Approved for COVID-19
- 10% bleach in water
- 70% ethanol
Disinfectant Contact Time
Disinfectants require a specific contact time in order to work. The majority require that you spray until the surface is thoroughly wet, then wait 5-10 minutes before wiping. If your disinfectant doesn’t have the specific contact time instructions on the label, that information should be available online.
- Do you have new muscle aches not related to another medical condition or another specific activity (e.g. due to physical exercise)?
- Do you feel like you may have a temperature of greater than 100.0°F?
- Do you have sore throat not related to another medical condition (e.g. allergies)?
- Do you have a new or worsening cough that is not related to another medical condition?
- Do you have shortness of breath that is not attributable to another medical condition?
- Do you have recent (less than five days) loss of smell and taste?
- Do you have new onset of vomiting or diarrhea not related to another medical condition?
- Have you had recent close contact with someone who has tested positive for COVID-19?